This article has a purely informative and educational role. It summarizes the different treatment options in the management of peri-implantitis. The article also gives a brief description of the etiopathogenesis, clinical features and the diagnosis of peri-implantitis to help the implantologist in his treatment decision.
This article should not be a source of remote diagnosis.
In this article we will discuss the causes of peri-implantitis, the means to counter and treat dental implant rejection and the possibilities of replacing a dental implant affected by peri-implantitis. Basal implantology is not affected by this disease since, thanks to its smooth surface, it allows you to rule out and does not suffer from peri-implantitis.
Rejection and infection of a dental implant
Peri-implantitis may be related to periodontitis or an infectious oral disease-causing soft tissue inflammation and bone loss. However, the latter concerns a dental implant but not a tooth. The origin of the infection is caused by the design of the implant, its degree of roughness or the design of the prosthesis overloading the implant. Families of microorganisms: Gram-negative anaerobes and spirochetes.
One of the other factors of dental implant failure is the breakage of the fixation screw in the implant. Once the screw is broken, the implant must be changed.
No rejection in basal implantology
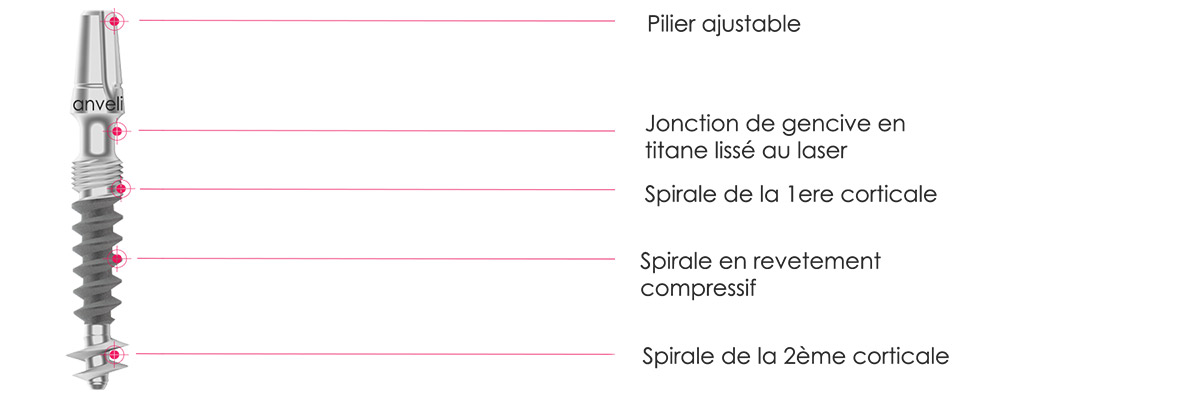
The failure of a dental implant is most often linked to a failure of osseointegration and a defect in loading. However, BAx (basal) strategic implantology is not based on osseointegration of implant but on a mechanical retention in the cortical zone. The dental implant being smoothed, the bacteria cannot find there a favorable ground for their development. This does not mean that there is no rejection in basal implantology. Other causes of rejection can be observed on small segments, the failure rate remaining lower during complete restorations. As this article is devoted to peri-implantitis, new generation basal implantology (BAx) will not be mentioned.
The other technological advance of the basal implant is its fixation by ceramic cementation. This makes it possible to avoid one of the frequent complications in traditional implantology: the breakage of the fixation screw.
As Prof. Ihde indicates in the video below, the strategic basal dental implant acts like other dental implants used in trauma surgery. There is no peri-implantitis if the latter keeps its stability.
Rejection (peri-implantitis) of a traditional dental implant

The term peri-implantitis refers to pathological inflammatory changes that occur in the tissue surrounding a rough-surfaced dental implant (traditional implant). The concept of peri-implantitis describes two entities: peri-implant mucositis and peri-implantitis. Peri-implant mucositis is defined as a reversible inflammatory reaction in the soft tissues surrounding an implant. Peri-implantitis is an inflammatory reaction with loss of supporting bone in the tissues surrounding the implant. In (traditional) crestal implantology peri-implantitis occurs in 5% to 8% of implants placed against 0.01% in basal implantology.
Loss of a dental implant
A dental implant is considered damaged if it is lost, mobile or if it has a peri-implant bone loss greater than 1.0 mm the first year and greater than 0.2 mm one year later. Peri-implantitis in most cases results in bone loss around the implant and total rejection in 90% of cases. Treatments for peri-implantitis have a low success rate around 10%. They will count the regeneration of the soft and hard tissues around the implant.
The causes of peri-implantitis
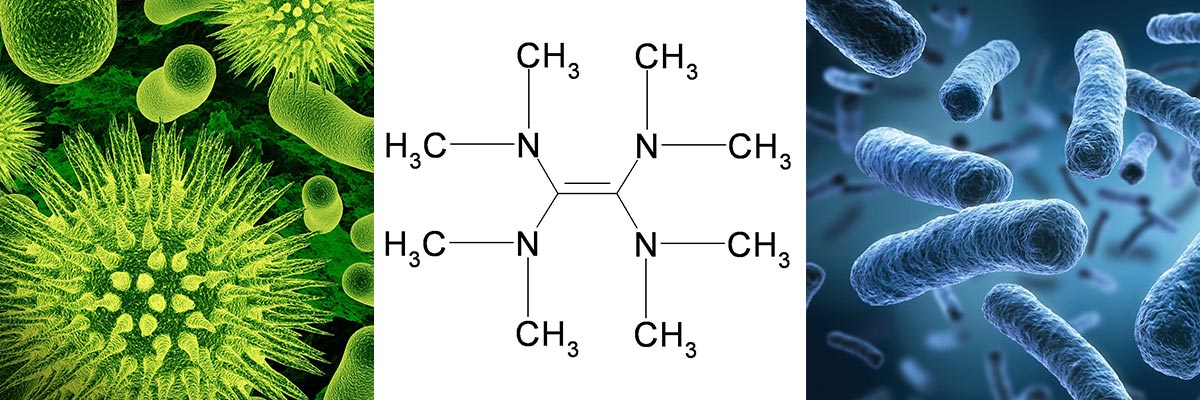
Bacterial infections play the most important role in dental implant failure. Dental implants attach themselves to the rough surface of the traditional dental implant. This rough surface is originally designed for tissue attachment. Bacteria associated with periodontitis and peri-implantitis show similarities. The microorganisms most commonly associated with implant failure are gram-negative anaerobes, such as Prevotella intermedia, Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans. Bacteroides forsythus, Treponema denticola, Prevotella nigrescens, Pepto streptococcus micros and Fusobacterium nucleatum.
Healthy peri-implant tissues play an important role as a biological barrier against some of the agents responsible for peri-implant disease and, if this is destroyed, bacterial contamination spreads directly into the bone, resulting in its rapid destruction. Excessive mechanical stresses, poor implant design and corrosion that can occur when a non-noble metal structure is connected to a titanium implant are important factors in the appearance and failure of the implant. development of peri-implantitis. Other factors include diabetes, osteoporosis, smoking, long-term treatment with corticosteroids, radiotherapy or chemotherapy.
Smoking is also considered to be an aggravating factor in peri-implantitis but only on traditional dental implants.
Diagnosis of peri-implantitis
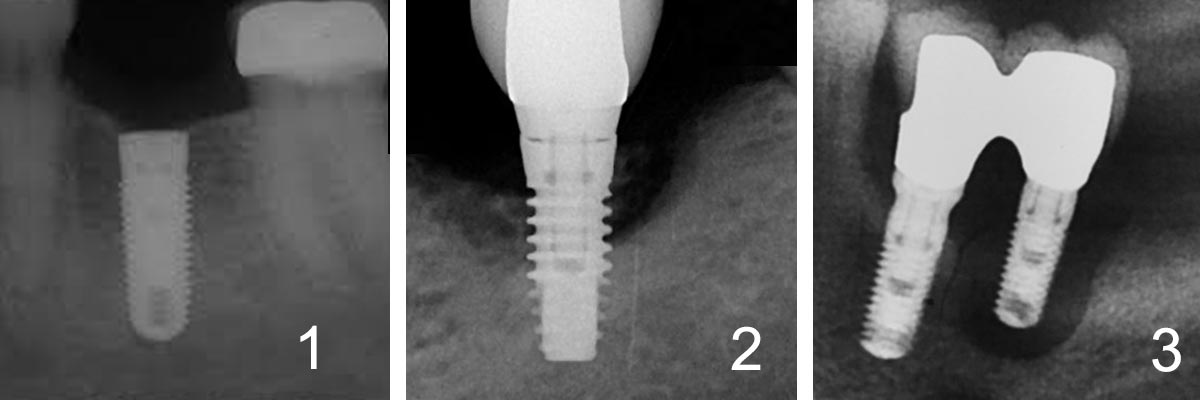
The above symptoms are typical of peri-implant and medium-term dental implant loss:
- Vertical destruction of cancellous bone. The defect is generally saucer-shaped and there is osseointegration of the apical part of the luminaire
- Vertical bone destruction associated with the formation of a peri-implant pocket
- Bleeding and suppuration on probing
- Possible swelling of the peri-implant tissues and hyperplasia
Pain is not normally present. If it is, it is usually associated with acute infection. The diagnosis of peri-implantitis requires careful differentiation from peri-implant mucositis, failures primary tissue integration and problems void of an inflammatory component. Diagnostic parameters used to assess peri-implantitis include clinical clues, peri-implant probing using a rigid plastic probe
Possible treatments for peri-implantitis
The treatment will strongly depend on the stage of advancement of the peri-implantitis. The greater the resorption, the rougher the surface is external to the bone tissue, the lower the chances of successful implant treatment. the dental implant will often be the preferred solution.
Local debridement
The implant should be cleaned using soft instruments such as polishing with a cup and rubber paste, dental floss, interdental brushes or using plastic scaling instruments. In fact, metallic and ultrasonic scalers can roughen the surface of the implant and increase the adhesion of bacteria.
The Karring & All study demonstrated that submucosal debridement, performed using an ultrasound device or carbon fiber curettes, is not sufficient to decontaminate the surface of implants with peri-implant pockets larger than 5mm when the rough implant surface is already apparent. So, it seems that mechanical or ultrasound debridement alone may be a solution only for primary stage peri-implantitis.
Decontamination of the implant surface
Four methods for decontaminating the surface of implants were compared on guinea pig monkeys:
- Air powder abrasive technique followed by application of citric acid
- Air powder abrasive technique
- A gauze soaked in a saline solution followed by an application of citric acid
- A gauze impregnated alternately with 0.1% chlorhexidine and physiological serum
The results of this study did not reveal any significant difference between the methods used. The results of an in vitro study combining photosensitization to toluidine blue solution and mild laser irradiation indicated that it was possible to eliminate bacteria from different titanium surfaces without modifying the implant surface.
Non-surgical treatment of peri-implantitis lesions using an erbium-doped laser has shown satisfactory results one month after treatment. According to Schwarz et al.
Anti-infective treatment
Studies regarding the presence of pathogens are essential in making a decision on antibiotic administration. Although the composition of the subgingival microbial component is important for drug selection, drug profiles oral administration are also important in deciding whether an antibiotic should be administered topically or orally. To make this decision, the doctor should examine the periodontal condition of the residual teeth.
The study by Schwarz showed that the treatment of peri-implant infection by mechanical debridement with plastic curettes combined with antiseptic treatment (0.2% chlorhexidine) could lead to statistically significant improvements bleeding after 6 months A study by Renvert demonstrated that adding antiseptic therapy to mechanical debridement did not confer additional benefit if the peri-implant lesion was greater than 4 mm. Localized implants, in the absence of other infections may be appropriate for local application of antibiotics by the insertion of tetracycline fibers for 10 days.
If peri-implantitis is present in several areas or if it is associated with periodontitis, a microbiological collection must be carried out and antibiotics administered systemically. Prof. Lang and his collaborators recommend: Systemic ornidazole 500 mg per day for 10 days or 250 mg of metronidazole per day for 10 days or a daily combination of metronidazole 500 mg and amoxicillin 375 mg every 10 days.
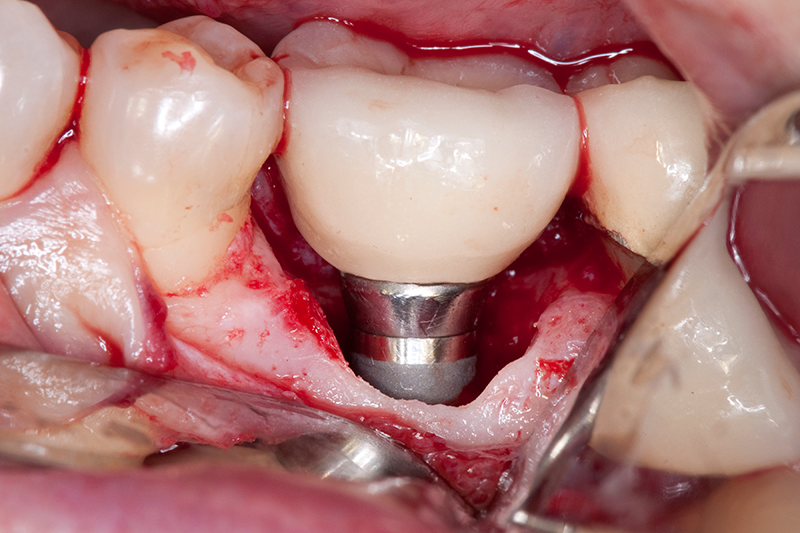
Surgical technique
Surgical treatment is generally limited to implants placed on non-aesthetic areas. The surgical flap technique helps complete debridement and decontamination of the implant affected by peri-implantitis. Surgical treatment is performed using autogenous bone grafts + membranes or membranes alone or even autogenous bone grafts alone.
However, the use of porous membranes can lead to bacterial penetration and lead to infection. Still there are no viable organism-controlled clinical trials to be available on the use of flap surgery. ‘Access only (debridement of the open flap) for the treatment of peri-implantitis.
Replacement of a dental implant after a rejection
The loss or the rejection of a dental implant has serious consequences on the bone volume present on the jawbone. Indeed, not only the peri-implantitis will have resulted in a melting of bone tissue but the volume of the (traditional) dental implant itself is substantial. Also, it is necessary to understand the causes of peri-implantitis. If these are not precisely established, replacing the dental implant with the same type of dental implant will present the same risks or even higher risks since in a good number of cases, a bone graft or a sinus lift will have been necessary.
Immediate replacement with the BAx basal implant
Basal implantology is used to treat patients who have suffered a rejection or loss of dental implant. With a basal dental implant, the risk of rejection is close to 0. We can thus in a single step, remove traditional dental implants with peri-implantitis and replace them directly with a BAx, BCS, BOI and KOS basal implant (strategic implant) . Thanks to its ultra-smooth titanium structure, and its mechanical retention, the risk of rejection is almost non-existent and it is not necessary to perform a bone graft.
Conclusion
The prognosis of a dental implant affected by peri-implantitis will depend on the detection and early treatment of the latter. Although studies of different treatment modalities for peri-implantitis are not comparable, it is believed the success rate of these treatments is low compared to the treatment time to be implemented. We recommend that dental surgeons inform the patient about all the possibilities and possible variations.
The solution of the basal implant, will be recommended when the complete quadrant must be treated in particular on patients at risk (smokers, diabetes …). If only one or two teeth must be treated with the presence of abutments, we recommend the installation of a bridge when possible.