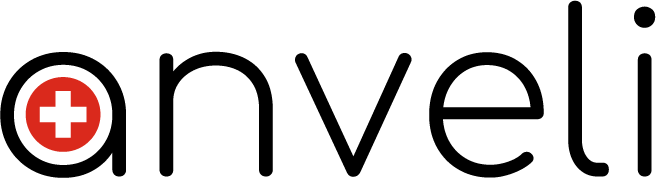
The jawbone is made like all the bones of the human body. It is made up of two kinds of bone:
Cortical bone:
Also called basal part which is the most mineralized and hardest part.
The spongious bone:
Inner part of the bone which, as its name suggests, resembles a sponge. This is the part that gives flexibility to the bone acting as a shock absorber.
Spongious bone
Cancellous bone is the inner part of the bone. It has a metabolic function with cells that are born and die. It is constantly renewed as long as the latter functions. In fact, when the latter loses its function (forces exerted from the tooth) the latter atrophies. The cells no longer have a reason to renew themselves. Cancellous bone also has an osteo-integrating effect. (The traditional implants are intended to be implanted in this spongy part, they consist of a rough surface that will allow them osseointegration). The cells will come to reconstitute themselves (it is sometimes said to heal). Like a metabolism, it can integrate or reject. Like a living being, it is difficult to predict its reaction. The cancellous bone acts as a shock absorber.
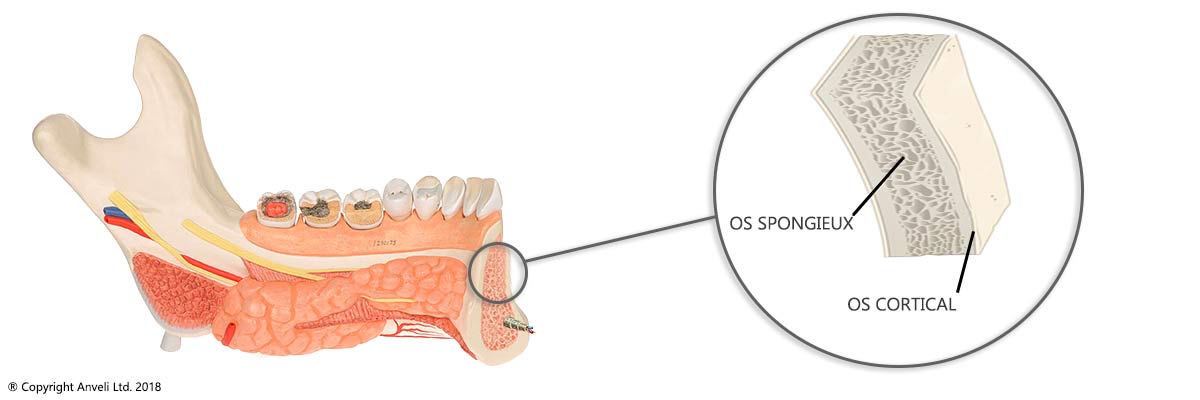
Bone regeneration
The bone, through its spongy (or crestal) part, is subjected to a constant regeneration process. Some cells synthesize the mineral base of bone and others eliminate old tissue. This regeneration slows down or ends when it stops to exist. There is no longer enough bone tissue or when the bone is no longer under stress such as after tooth loss.
Cortical bone
The cortical bone (where the basal implant is placed) has a mechanical function. It is present in lesser quantity on the bone but retains an almost constant volume. It is a fabric that has greater mechanical resistance and greater density. It is located at the back of the mouth at the location of teeth 7 and 8 and in the nasal area (1, 2 and 3) for the upper jaw and on the entire lower jaw. It does not have an osteo-integrative function. (Basal dental implants have a smooth surface because it is their shape that allows the attachment and maintenance of the implant.)
To understand the constitution of the maxillofacial bone, one must also understand the elements that accompany it. Namely, the joint, soft tissue, sinuses and nerves. Each element has an interaction with / against others.
Bone loss and atrophy

Bone tissue retains all of its qualitative and quantitative characteristics when stimulated by force. This force can be transmitted by a tooth or by an implant. When a tooth is extracted and not not replaced by a dental implant, in this case a natural phenomenon occurs. The jawbone will undergo bone resorption leading to bone atrophy (deficit).
The resorption of the bone occurs in a different way on the upper jaw and on the mandible. It can be aggravated by wearing a removable prosthesis, an All on 4 type prosthesis or by a peri implantitis.
Bone atrophy can reach 5 to 6 millimeters the first year (hence the advantage of immediate implantation post extraction) then 1 to 2 mm per year.
On the upper jaw bone loss acts both from below up along the roots and both from above with the sinus floor growing on the bone. there is no more tooth or implant to hold it, it can then descend until it leaves only the thickness of a sheet of bone tissue paper. Bone atrophy also acts in thickness.
Dental implants (traditional) can also negatively affect bone tissue when peri-implantitis occurs.
Bone grafting makes it possible to regain bone height by performing it immediately after extraction. Since its implementation in the 1980s, bone grafts have undergone many improvements. There are several techniques depending on the location. An increase in bone in the sinus cavity is called a sinus filling or sinus lift. An increase in height or thickness is called a shuttering or apposition graft. However, these interventions are carried out less and less since the arrival of the basal techniques making it possible to avoid the bone graft.